News
Updates
NYMDA PUBLIC POLICY COMMITTEE UPDATE
The NYMDA Public Policy Committee continues to be active and build an ongoing legislative relationship with the Medical Society of the State of New York (MSSNY). NYMDA has submitted 2 resolutions at the MSSNY House of Delegates over the last 2 years. Both were approved and accepted by the house. Once a resolution is accepted it becomes a part of the state medical society's legislative agenda for advocacy with New York State. The 2 resolutions that were passed involve the establishment and maintenance of a medical director registry as well as establishment of a regulatory database in Assisted Living Facilities. Both are significant issues that can impact medical directors but also impact healthcare delivery at a system level.
MSSNY HOD 2021
Nursing Home Medical Director Registry
Introduced by MSSNY Young Physician Section, Monroe County Medical Society
Seventh District Branch
ADOPTED
RESOLVED, that MSSNY collaborate with the New York State Department of Health to create an active/up to date registry for nursing home medical
directors and associate medical directors, that can easily be accessed by physicians, hospitals, and/ or health systems.
MSSNY HOD 2022
RESOLUTION 103 - ASSISTED LIVING RESIDENCE (ALR) NYS REGULATION
Original Resolution 103 Reads as Follows:
RESOLVED, that MSSNY with the support of the NY Medical Directors Association (NYMDA), collaborate with the New York State Department of Health to create an easily accessible database which would make all Assisted Living Residence (ALR ) rules, regulations and links to Dear Admin Letters (DALs) available to staff at assisted living facilities, primary care provider teams, hospitals, and/or health systems and which would be updated when appropriate.
RECOMMENDATION A: THE REFERENCE COMMITTEE RECOMMENDS THAT THE FOLLOWING SUBSTITUTE AMENDMENT BE ACCEPTED INSTEAD OF ORIGINAL RESOLUTION 103:
RESOLVED, that MSSNY with the support of the NY Medical Directors Association (NYMDA), collaborate with the New York State Department of Health to create an easily accessible database which would make all Assisted Living Residence rules, regulations (ALR) and links to Dear Admin Letters (DALs) available to staff at assisted living facilities, primary care provider teams, hospitals, and/or health systems and which would be updated when appropriate at least annually.
RECOMMENDATION B: THE REFERENCE COMMITTEE RECOMMENDS THAT SUBSTITUTE RESOLUTION 103 BE ADOPTED
UPDATED REQUIREMENTS FOR CME RECERTIFICATION AND REINSTATEMENT:
The American Board of Post-Acute and Long Term Care Medicine (ABPLM) is changing the requirements for recertification and reinstatement. It is important to the quality of care in the nursing home to have a knowledgeable and skilled medical director. As more physicians have dedicated their careers to the long term care continuum the opportunities for physician to lead and improve the care provide have grown. In order to acknowledge the importance of physician with expertise in medical direction serving in industry leadership roles the ABPLM is expanding the experience requirement to include those holding a leadership position that influence the care provided by the medical providers. With this change medical directors that transition to a role that is not the medical director of a particular nursing home, but the role still involves leading clinical medical providers in the long term care continuum. This type of leadership role will meet the experience requirement for recertification and reinstatement as a certified medical director.
The process of reinstatement as a Certified Medical Director changed to remove barriers to restarting the certification process. The recredentialing and reinstatement process will now be the same. For the educational requirement, the medical director must have 60 clinical CME and 60 management credits within the last 6 years. The experience requirement will be the same of having served in a clinical leadership role in the long term care continuum within the last 6 year. There will no longer an additional $100 fee for reinstatement.
The change to expand the types of roles that count got the experience requirement and the elimination of the barrier to reinstatement are an effort to acknowledge the changing long term care industry. ABPLM feels these changes will help to keep knowledgeable engaged physicians working to grow their skills in medical direction.
Posted 3/2/2022
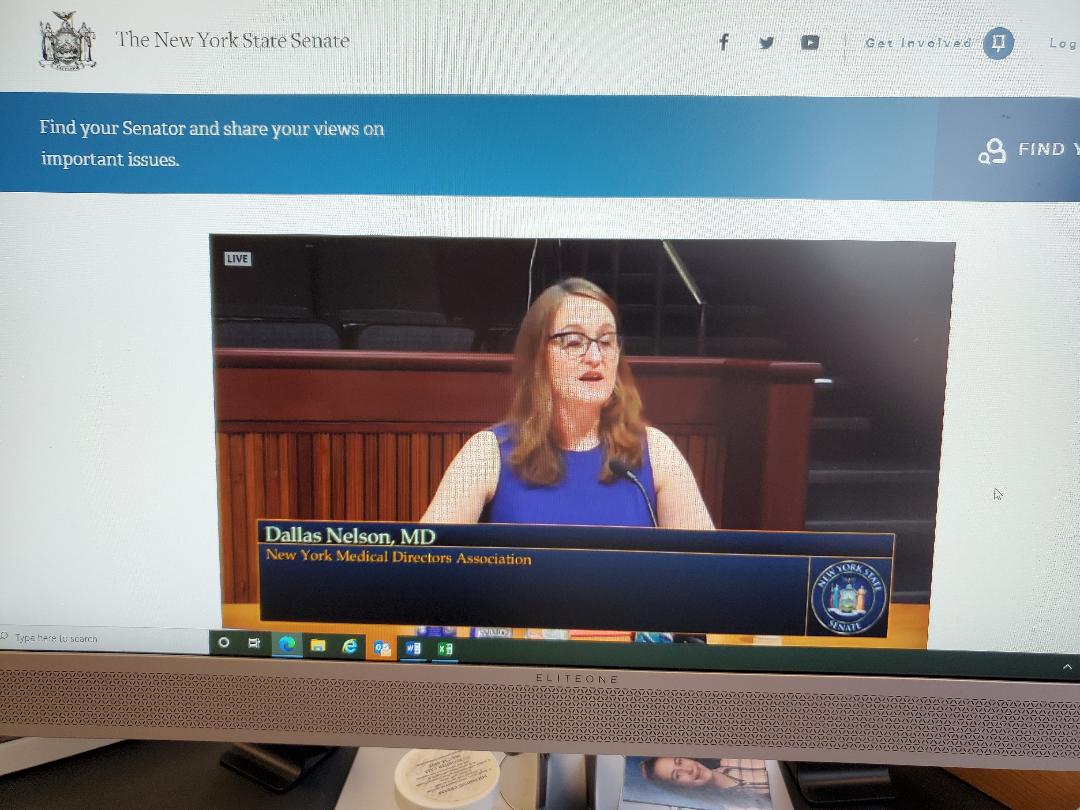
Dallas Nelson, MD, FACP, CMD - President of NYMDA - Provided Oral Testimony at the NYS Senate Committee on Aging on 7/27/21
Greetings. I’m Dallas Nelson from Rochester, NY and representing the New York Medical Directors Association, an organization who goal is educating and advocating for long term care medical directors and medical providers. I’m also the medical director of 2 nursing home and 2 assisted livings, one the nursing homes that served as a designated COVID 19 positive unit for the state. I provide primary care provided across the long term care continuum, and I am the granddaughter of a nursing home resident. An engaged, knowledgeable medical director can improve a facility’s system of care with the application of science to care. Medical directors need to be expert in the discipline of quality assurance and process improvement or QAPI. From QAPI we know that systems generally get the outcomes that they are designed to produce. The long-term care system is currently producing a severe shortage of front-line workers, namely nurses and CNAs. Society will be judged by the quality of care we provide to our most vulnerable members.
Before COVID, the staffing levels in some of my facilities was below what was needed to properly care for the residents. The staff was chronically stressed because they were covering more work than they could do. The long-term care industry is plagued by frequent turnover of the staff and even leadership. Then COVID 19 made nursing homes the hotspot for the most serious outcomes of the pandemic. In my nursing homes each surge of the pandemic decreased the staffing further, worsening our ability to respond to the next outbreak. Last year working in the nursing home became one of the most dangerous jobs in America. The rate of death for nursing home workers was higher than that of the logging industry. Frankly the long-term care facilities became environments of overwork, fear, and danger.
I can write state of the art geriatric medical plans for Ruth, but if no one is there to complete the plan it doesn’t matter. As a society we are paying in human suffering for the current long-term care system. Our parents and grandparents are suffering from staff shortages and as a result a greater incidence of falls with facture, death secondary to failure to thrive, and skin breakdown.
This problem is not a result of laziness or greed. Quality improvement teaches that searching for bad apples is less likely to result in widespread positive change. More effective is to bring together the people with deep knowledge of the system, front line workers, and those who control resources and regulations to systematically study the root causes of the problems and design interventions to fix the system.
The pandemic highlighted how intertwined all the sights of healthcare are with each other, including nursing homes, assisted livings, home care, and the hospitals. The healthcare system needs patients to move through the nursing homes after hospitalization to gain the ability to function in their own home. Each of these levels of the healthcare system is needed to serve the entire compliment of vulnerable people and they are competing for a similar finite pool of resources. The New York Medical Directors Association felt that Reimagining Long Term Care Task Force was a good first step. The bill was one of the first opportunities for the long-term care medical directors to have a seat at the table to use our expertise in long term care medicine to advocate for our patients. While it may be too late for that bill, we do hope for legislation to spur on the start of the effort to improve and redesign the long-term care system. The Colorado Medical Directors Association regularly meets to collaborate with their Department of Health. NYMDA would like an open, collaborative relationship with to Department of Health to work to improve the care of New York’s vulnerable elderly. Our hope is that the stakeholders responsible for the care of the older adults will work collaboratively to improve the system.
CMS Announces Changes to SNF/ALF Provider Reimbursement: 12/2020
The New York Medical Directors Association and the Society for Post-Acute and Long-Term Care Medicine strongly opposes policy the Centers for Medicare & Medicaid Services (CMS) finalized on December 1, 2020, to cut payments for evaluation and management (E&M) services in nursing facilities, assisted living, and home health by nearly 10% effective January 1, 2021.
Physicians, nurse practitioners, physician assistants, and occupational/physical therapists who practice in these settings have put themselves at the highest risk caring for patients who have been the hardest hit by the COVID-19 pandemic. These clinicians face incredible physical and mental hardship, as many are forced to isolate from their families and suffer the consequences of contracting the virus themselves. Cutting these services at this time is simply unconscionable.
We are asking you to Contact Your Members of Congress to ask them to waive the budget neutrality requirements stipulated in Section 1848(c)(2) of the Social Security Act before the final E/M code proposal is implemented on January 1, 2021.
See more through links below:
Full article is available here
ACT NOW: Contact your elected officials by clicking here